How is colposcopy performed?
A colposcope is a microscope that resembles a pair of binoculars. The instrument has a range of magnification lenses. It also has color filters that allow the physician to detect tiny abnormal blood vessels on the cervix. The colposcope is used to examine the vaginal walls and cervix through the vaginal opening.
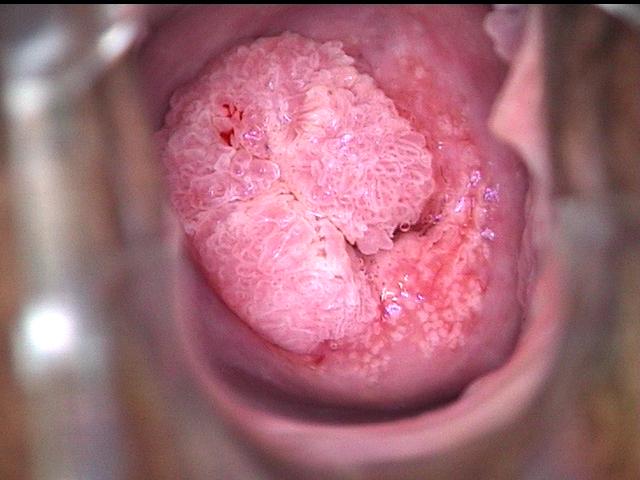
- The first step of the procedure is examining the vulva and vagina for signs of genital warts or other growths. (Genital warts are caused by the human papilloma virus (HPV), which is a sexually transmitted virus that causes cervical cancer).
- A Pap smear is then taken.
- The cervix is inspected and special tests are performed.
Colposcopy is a safe procedure with no complications other than vaginal spotting of blood.
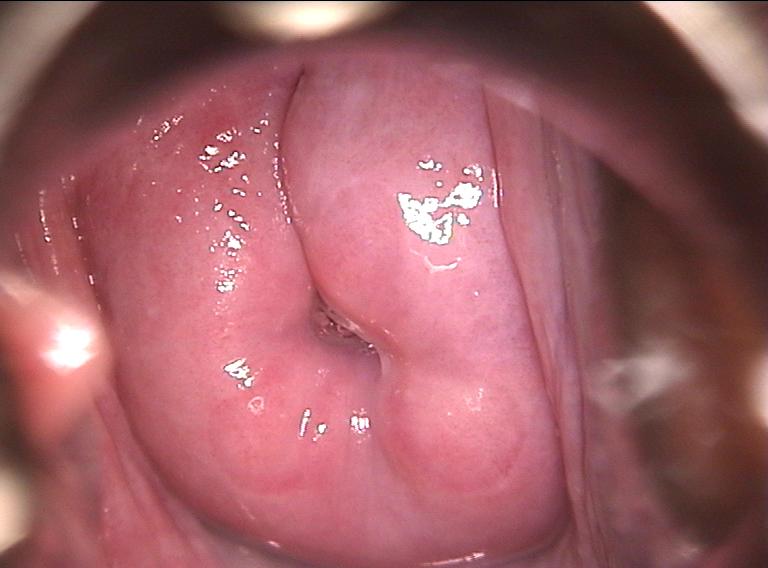
The examiner wants to get a good look at the squamocolumnar junction, which is the area of the cervix that gives rise to most cases of cervical cancer. The term squamocolumnar junction refers to the border between the two different types of cells (squamous cells and columnar cells) that normally form the lining of the endocervical canal. (This canal connects the cervix with the main part of the uterus.) Most cases of cervical cancer originate from the squamous cells and, therefore, are referred to as squamous cell cervical cancer.
Which special tests are performed during colposcopy?
Three special tests are done during colposcopy: acetic acid wash, use of color filters, and sampling (biopsy) of tissues of the cervix.
1. Acetic acid wash
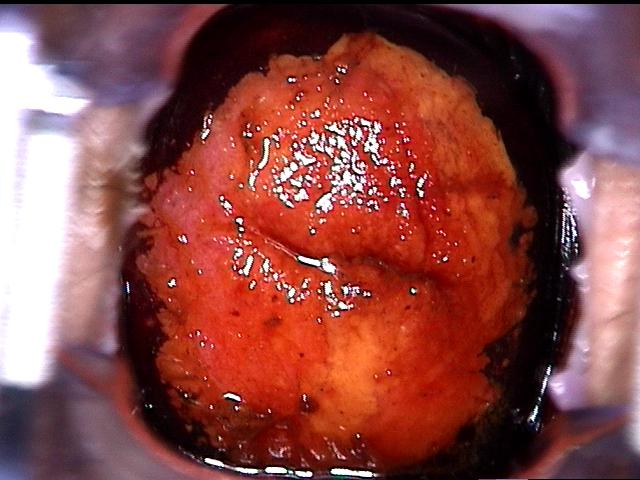
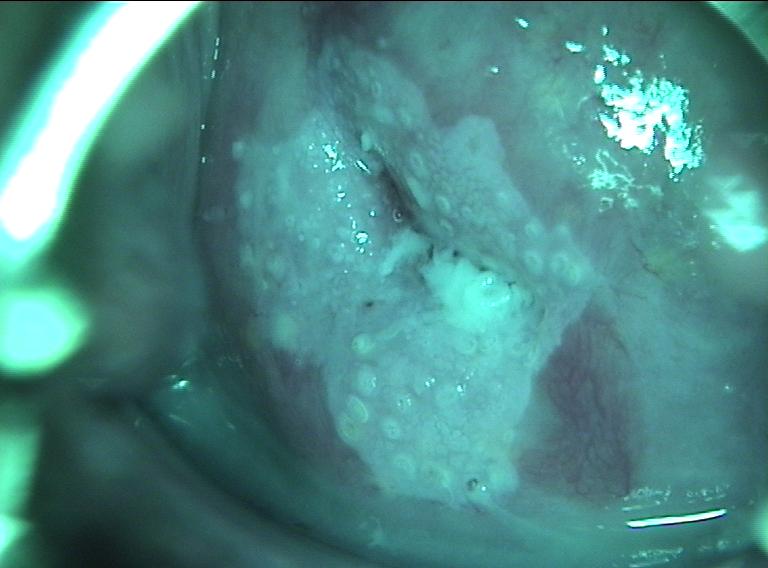
After the cervix is studied with the colposcope, the cervix is washed with a chemical called 3 – 5% acetic acid. The acetic acid dissolves mucus and stains the abnormal areas white. (acetowhite lesions). Staining with a dilute iodine solution (known as Lugol's solution or Schiller's solution) is also performed to further examine for abnormalities. Normal cells will generally take up the iodine stain (and turn brown) in a uniform manner, whereas severe precancerous and cancerous areas will not.
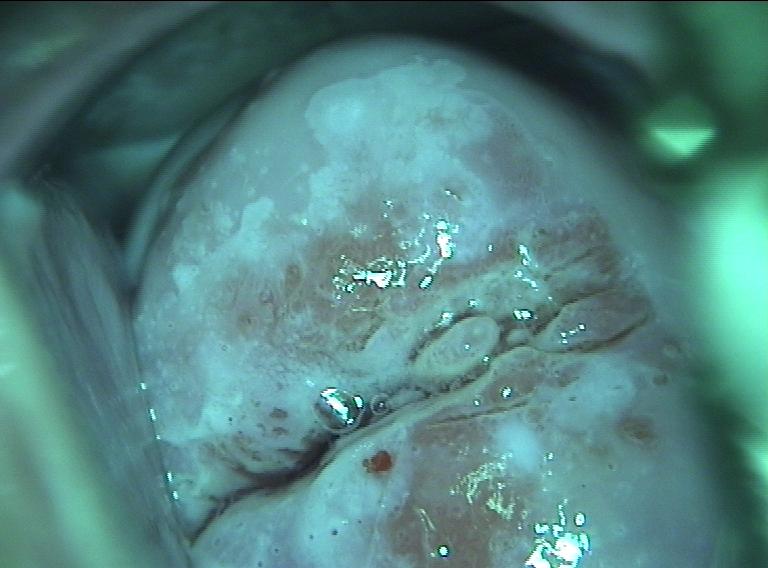
2. Use of color filters
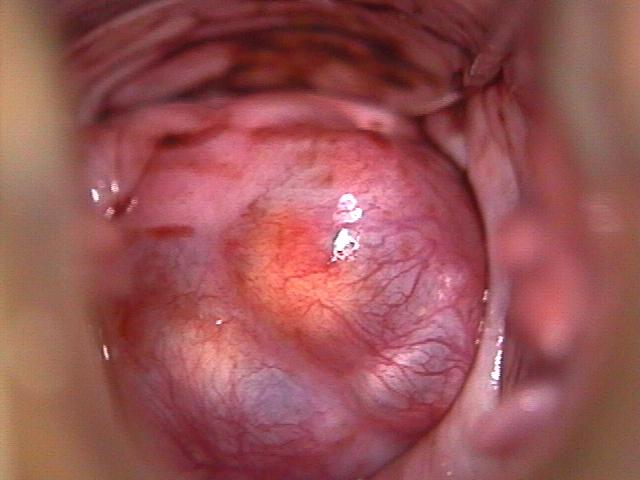
Color filters help the physician examine tiny blood vessels (capillaries) in the area of the squamocolumnar junction. Blue or green filtered light can cause abnormal capillaries to become more obvious, usually inside an acetowhite area. Normal capillaries are slender and spaced out evenly. In contrast, abnormal capillaries can appear as red spots (thickened capillaries seen on end) or can produce a pattern resembling hexagonal floor tiles.
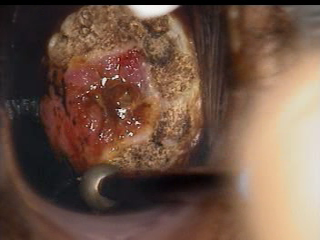
3. Biopsy of the cervix
Colposcopy allows tissue sampling (biopsy) that is targeted to the abnormal areas. In fact, the biopsy of abnormal areas is a critical part of colposcopy because treatment will depend on how severe the abnormality is on the biopsy sample.
Based on the colposcopy results, what is the approach to treating cervical abnormalities?
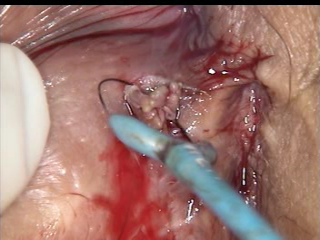
If the biopsy results show pre-cancer (dysplasia) or cancer, treatment is recommended. The dysplasia may be mild, moderate, or severe. Almost all women with dysplasia can have their treatment procedures performed in the doctor's office. The physician chooses between two general types of treatment. The first type is destruction (ablation) of the abnormal area, and the second type is removal (resection). Both types of treatment cure 90% of patients with dysplasia, meaning that 10% of women will have a recurrence of their abnormality after treatment. Generally, destruction (ablation) procedures are used for milder dysplasia and removal (resection) is recommended for more severe dysplasia or cancer.
The destruction (ablation) procedures are electroablation and cryocautery. The removal (resection) procedures are loop electrosurgical excision procedure (LEEP), cold knife conization, and hysterectomy.